Automating workflow processes
Imaging centers are targeting both internal and external workflow to gain significant improvement in service delivery and, at the same time, making progress toward the realization of the electronic health record.
Workflow improvements also are proving to decrease operational costs. Making this possible are new alternatives available to imaging centers that offer the option of a more proactive, efficient and profitable planning and design process.
Advancements include:
- Delivering reports electronically to the referring physician’s Electronic Medical Records (EMRs) system to increase customer satisfaction and retention
- Combining patient, clinical and image data into a consolidated view that enhances the radiologist’s read process and improves productivity
- Automating and integrating both coding and billing, thereby increasing reimbursement and decreasing operating costs
The impact of a modern workflow, when orchestrated properly, quickly results in improved service delivery, greater customer loyalty, the capture of new business, and efficiencies which improve profitability.
In the past, radiology workflow has been dictated by its applications. Manual processes were developed to support limited technology and compensate for the gaps between systems. Today, it is becoming more common to design an optimal workflow model and expect technology and supporting applications to accommodate it.
Challenges of traditional radiology workflow
The challenges of traditional radiology workflows are evident in the following areas:
- Exchanging information with referring physicians
- Radiological interpretation process
- Billing and coding process
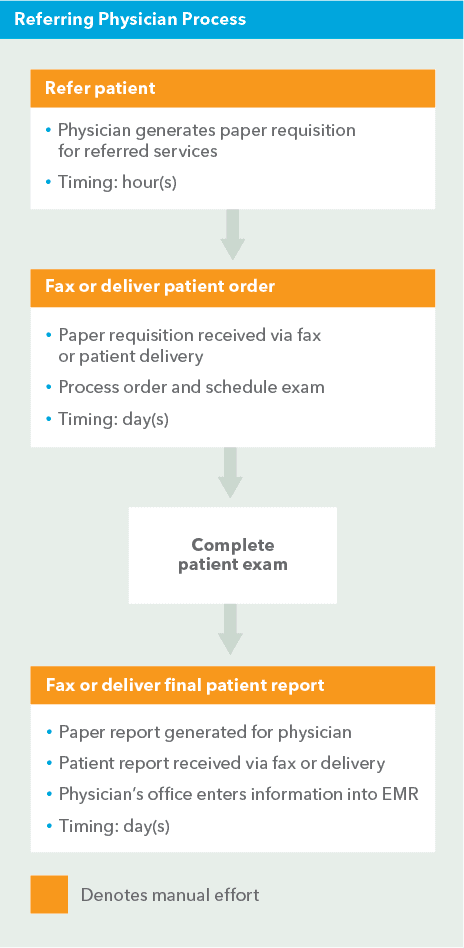
Exchanging information with referring physicians
Manual processes are often the limiting factor in turnaround time and delivery of reports.
When a paper order is received by an imaging center, it is typically physically processed, often in a staging room. The patient is designated as “new” or “returning” and their demographic information is entered or updated in the appropriate applications. During and after the patient visit, correlating patient data, images, and reports is mostly a manual effort which delays the delivery of the patient report.
At the end of the process, a patient report is delivered to the physician who must then manually enter the data into their EMR system, taking valuable time and creating a higher probability of entry error. These manual-entry inefficiencies are then passed on throughout each step of the workflow.
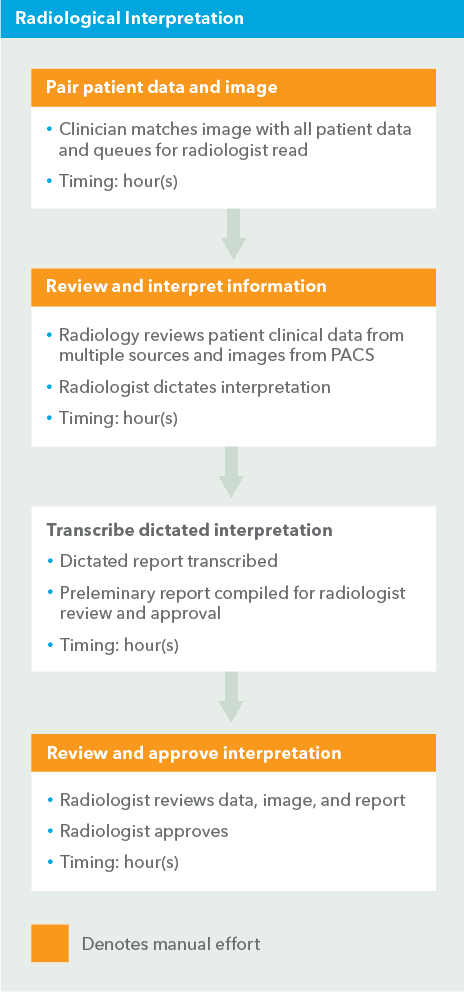
Radiological interpretation process
In a practice that employs state-of-the-art imaging technology, doctors are often continuing to shuffle through papers to find the information they need. While adopting a Picture Archiving and Communication System (PACS) solution is widely viewed as critical to improving the workflow, other technology advances are commonly ignored. In many instances, supporting clinical information is only available as a paper document. The radiologist, as a result, juggles digital images, papers, and dictation equipment.
This type of workflow severely limits a radiologist’s mobility at a time when many imaging centers have multiple locations that provide professional services for hospitals and other facilities. Sub-specialization poses an even greater challenge to provide the right expertise for each patient in a timely fashion.
Billing and coding process
The cost, in terms of man-hours and paper use, involved in billing across multiple facilities and organizations is immense. All of the billing systems involved have to accommodate the “lowest common denominator” in the process. Consequently, fulfilling the requisition for demographic and insurance information usually requires paper records to be manually retrieved from multiple applications.
As outlined in the three processes above, each manual step contributes to a longer turnaround time for reports, resulting in a profound impact on the patient’s experience and referring physician and radiologist satisfaction. When paper is the only item connecting a patient/physician with an outpatient imaging center, continuity of care is often limited.
Solving workflow challenges
Understanding the steps required to obtain the desired result is the key to streamlining these three processes:
- Exchanging information with referring physicians
- Radiological interpretation process
- Billing and coding process
After the workflow is understood and documented, applying technology to automate key steps will quickly help reduce cycle time and increase overall effectiveness.
Electronic data exchange with referring physicians
Referring physicians are demanding a more efficient and cost-effective way to exchange patient information with specialized providers such as radiologists. Although creating a web portal to give a physician access to patient results is an option, it only partially addresses the problem and does not eliminate the required, mistake-prone and inefficient manual re-keying of information. Electronically integrating directly with the physician’s EMR is a complete solution to this problem.
Through an HL7 interface, patient demographics and order information may be sent directly to the RIS system from the referring physician. After the patient report is ready, the RIS sends the report directly to the physician’s EMR. Routine manual effort can be eliminated entirely. Key benefits include:
- Enhanced service levels Patient reports are delivered directly to the physician’s EMR. A material link between the referring physician and imaging specialist is established, resulting in quicker turnaround times and improved customer loyalty.
- Reduced operational costs Automation saves time by reducing or eliminating faxed physicians orders and results and also the re-keying of data.
- Reduced errors The opportunity for clerical errors is minimized with a decreased need to rekey data. Automation reduces or eliminates many of the manual data entry points.
Radiological interpretation workflow
This scenario starts with a filmless workflow but goes beyond implementing a PACS solution. It reflects integration between multiple applications and the ability of radiologists and clinicians to interact with an enterprise-wide dynamic worklist. Ideally, the radiologist would have the images and supporting documentation displayed and could begin dictation with a single click.
The RIS must feed the PACS critical patient data. If an imaging center has also implemented a voice recognition system and a document management solution, the RIS will provide relevant information to both. Although the RIS is a key source for patient information, a single-vendor approach is not required to accomplish the integrated workflow. HL7 interfaces can connect disparate applications to share data and drive workflow efficiencies.
Key benefits include:
- Increased radiologist productivity With integrated systems, a radiologist significantly reduces the time spent locating paper patient records during the interpretation process. Sign-off on the report can happen immediately, avoiding unnecessary requests for clarification and approval.
- Decreased cycle time, increased volume Optimizing the interpretation process decreases the turnaround time for reports and boosts the volume of completed reads. By adding electronic delivery, a report can be generated and sent to the physician before the patient leaves the facility, rather than hours or days later.
- Value added services While the imaging center stands to increase revenue by improving a radiologist’s productivity, the center can also provide more highly valued services. With automation, a radiologist can be matched to the patient’s needs regardless of the physical location of the procedure or patient.
Billing and coding processes
Billing for contracted professional services starts with integration to the Hospital Information System (HIS) or EMR of the referring facility. Through HL7 interfaces, patient demographics and reports can be sent directly to the RIS or may be routed elsewhere for use in insurance coding.
Electronic communication opens many opportunities to streamline this process. For example, after querying existing patient records with the desired criteria, the existing insurance information might be selected for billing. The entire billing process can be reduced to a few manual steps, such as coding and review of irregular records.
Key benefits include:
- Reduced operational costs Automating the billing process will eliminate complex and labor-intensive procedures. Depending on the size of the practice, FTEs may be recovered and leveraged in a more value-added role. Additional costs associated with processing, management and storage of paper-based billing transactions can also be eliminated.
- Decreased reimbursement cycle time, increased accuracy Each manual step eliminated or improved with automation contributes to decreasing the cycle time for reimbursement. Fewer touch points eliminates opportunities for re-keying errors. With automated workflow, tighter control of billing, patient and insurance data is achieved, thereby increasing the accuracy of claims.
Summary
The positive impact of automating workflows can be identified in many areas within a radiology practice.
Understanding and documenting your workflow will allow you to take advantage of recent advances in technology that facilitate workflow automation and optimization. The benefits are far-reaching:
- Enhanced delivery of care
- Increased productivity
- Greater customer satisfaction
Imaging centers offering electronic data exchanges will strengthen their reputation amongst referring physicians, and create a foundation able to support an expanding referral community and increased volume of business.
